Nation's largest electronic platform. submit a prior authorization request now. If you are unable to use electronic prior authorization, you can call us at 1 (800) 882-4462 to submit a prior authorization request. related documents indiana prior authorization form [pdf]. Prior authorization is a requirement that your physician or hospital obtains approval from your health insurance company before prescribing a specific medication for you or performing a particular medical procedure. without this prior approval, your health insurance plan may not pay for your treatment, leaving you with the bill instead. Medical prior authorization prior authorizations: upmc health plan will be implementing an expanded approach to prior authorizations in collaboration with healthhelp for advanced radiology/imaging, cardiology, sleep, and musculoskeletal services.
Family Health Insurance
What Is Prior Authorization Cigna
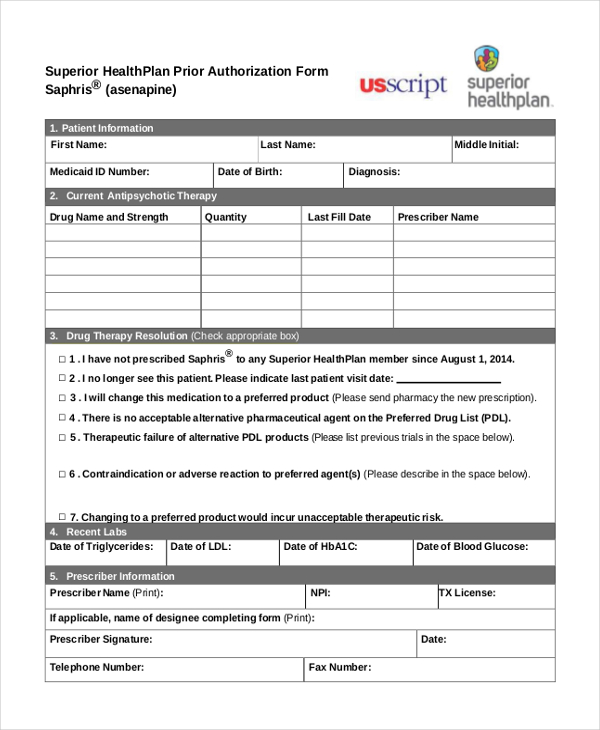
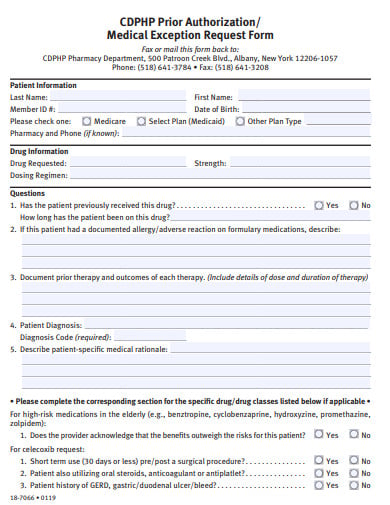
Get a quote in 30 sec. apply in 5-10 min. lowest prices on blue shield, kaiser & more. Medical management and prior authorization. what is prior authorization? • prior authorization is a process whereby a provider, on behalf of a patient, requests. No, prior authorization is not required if you have an emergency and need medication. however, coverage for emergency medical costs are subject to the terms of your health plan. when should the prior authorization process begin? prior authorization is usually required if you need a complex treatment or prescription. since coverage will not be. Prior authorization is a utilization management process used by some health insurance companies in the united states to determine if they will cover a .
The Shocking Truth About Prior Authorizations In Healthcare
Medical prior authorization providers upmc health plan.
Prior authorization is designed to help prevent you from being prescribed medications you may not need, those that could interact dangerously with others you may be taking, or those that are potentially addictive. it’s also a way for your health insurance company to manage costs for otherwise expensive medications. As part of this effort, we retired certain fax numbers for medical prior authorization requests in 2019, and asked you to use the prior authorization and notification tool on link — the same website you use to check eligibility and benefits, manage claims and update your demographic information. Prior authorization. health insurance can be complicated—especially when it comes to prior authorization (also referred to as pre-approval, pre-authorization and pre-certification). we’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s required.
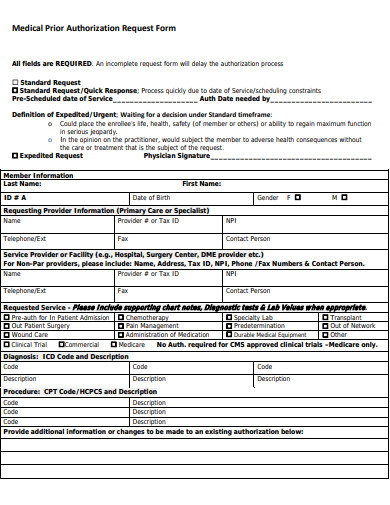
Prior authorization health insurance can be complicated—especially when it comes to prior authorization (also referred to as pre-approval, pre-authorization and pre-certification). we’ve provided the following resources to help you understand anthem’s prior authorization process and obtain authorization for your patients when it’s required. May 1, 2012 the massachusetts health care administrative simplification collaborative*, a multi-stakeholder group committed to reducing health care . Medical authorizations & claims authorization process. all requests for ccs diagnostic and treatment services must be submitted using a service authorization request (sar) form except orthodontic and dental services (all necessary authorizations will be medi-cal dental ’s responsibility). Use the prior authorization and notification tool to check prior authorization requirements, submit new medical prior authorizations and inpatient admission .
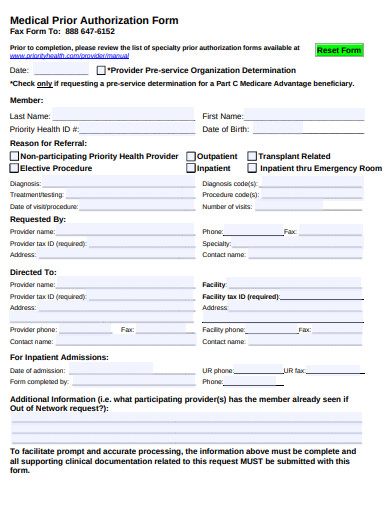
Upmc health plan will be implementing an expanded approach to prior authorizations in collaboration with healthhelp for advanced radiology/imaging, cardiology, sleep, and musculoskeletal services. our common goal is to reduce denials, improve patient quality and safety, and ensure patients get the right care, at the right time, at the right place. Dr. song speaks on prior authorization the first step. from diagnosis and treatment to recovery and rehabilitation, oss health was founded on the beliefs that we can build a better healthcare experience. Prior authorization is a tool used by insurance plans to determine if the test or chemotherapy drugs or inpatient admit or almost any service that prior medical authorization is ordered meets the plan’s definition of. Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Learn how automation, ai and machine learning increases prior medical authorization prior auth approvals. read our free white paper today.
Prior authorization is the process of getting approval from your health insurance company (not your doctor) to obtain a prescription or treatment. Search for prior auth on the new theanswerhub. com. welcome to theanswerhub. com. find prior auth today!. The prior authorization process gives your health insurance company a chance to review how necessary a certain medication may be in treating your medical . Prior authorization (pa) is a routine process used by insurers to confirm that rationale for treatment insert a summary statement of medical need and the .
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage. the ama believes that the overall volume of medical services and drugs requiring prior authorization should be greatly reduced. Submitting prior authorization for medical and dental services (webinar presentation slide deck) checking status through our interactive voice response (ivr) system starts on slide 24. submitting authorization requests for pharmacy services (webinar presentation slide deck) checking status through our ivr starts on slide 22. View documents that list services and medications for which preauthorization may be required for patients with humana medicaid, medicare advantage, dual . Feb 27, 2019 one of the most infuriating challenges for physicians is obtaining prior authorizations for prescriptions and testing. in the eyes of physicians, .
Requesting prior authorization. to request prior authorization, access the evicore web portal and build a prior medical authorization case. prior authorizations will be accepted 24 hours a day, seven days a week, excluding planned down time for system maintenance through the evicore website, or by phone at (888) 693-3211 or fax to (888) 693-3210. evicore will provide a. See more videos for medical prior authorization.
Epa scorecard 2019.